National Institute for Public Health and the Environment (RIVM) research: chance of contracting corona indeed smaller by keeping distance (retrieved from Dagblad van het Noorden, in Dutch). People who adhere to the advice to keep 1.5 meters distance from others, run less risk of contracting the corona virus. That is the outcome of a study conducted by the Dutch National Institute for Public Health and the Environment (RIVM). It shows that “social distancing is an important measure to stop the spread of the virus,” says the RIVM.
Infection rate 27 Percent lower by keeping social distance
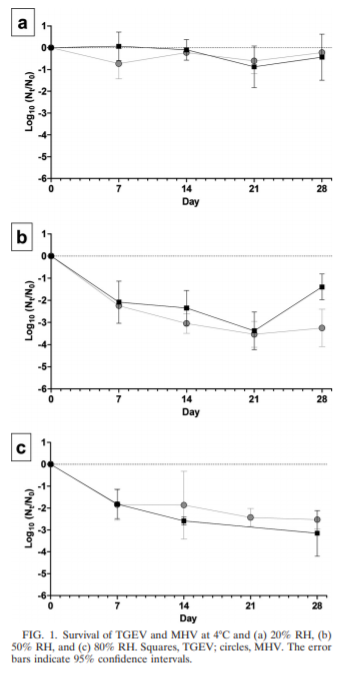
The researchers analyzed data from 7,000 people who filled out regular questionnaires about their contacts during the first corona wave. Their blood was also tested for antibodies, which can be used to show that someone has been in contact with the virus. At the time, 5.5 percent of the people who did not follow the distance rules had antibodies in their blood. Of the participants who said they did, 4 percent made antibodies. Thus, among those who kept their distance, the infection rate was 27 percent lower.
Large group meetings lead to more infections
Large group meetings also lead to more infections, the study shows. Of the people who indicated that they had attended a meeting in an indoor space with more than 20 people, 6.2 percent were found to have antibodies in their blood. That percentage was one and a half times higher than among people who indicated that they had not attended any meetings at all.
1 in 5 of blood donors have antibodies
Meanwhile, many more people have antibodies in their blood. A random sample from the Sanquin blood bank recently showed that this concerns more than one in five blood donors. Among them are also people who have been vaccinated.
The research results of the RIVM were published in the scientific journal Clinical Infectious Diseases. They also show that people who had particularly close contact with children under the age of 10 hardly became infected with the virus. “There were no more antibodies in the blood of these participants than in participants who indicated they had no contact at all.”
New virus variants, such as the British variant that is now dominant, did not exist when the study was conducted. “Precisely because of the higher infectivity of these variants, it is important to keep a sufficient distance,” says the RIVM.
Covid Buzzer helps to keep social distance
Social Distancing, wearing a mouth mask, proper marking and hand washing help prevent the spread of Covid-19. Solutions like the Covid Buzzer help maintain social distance.